High PSA - How Do I Find Out if I Have Prostate Cancer?
When is a Prostate-Specific Antigen (PSA) Done?
The PSA test is a blood test used for the early detection of prostate cancer. The test measures the amount of
prostate-specific antigen (PSA)
in your blood. PSA is a protein produced by both cancerous and noncancerous tissue in the prostate, a small gland that sits below the bladder in men.
Typically, the PSA test is done for men aged 50 and above who are concerned about prostate cancer. The PSA test may also be done for men who have urinary symptoms or have a family history of prostate cancer.
PSA for early detection of prostate cancer
Although the PSA test is prostate specific, it is not a prostate cancer specific test. Other non-cancerous conditions such as benign enlarged prostate, prostate inflammation (prostatitis) or recent urinary infection may also cause an elevated PSA. A PSA level 4.0ng/ml and above is considered abnormal, with a elevated risk of prostate cancer. Whilst a very high PSA (above 20ng/ml) is often associated with cancer, most men with high PSA will have a PSA in the range of 4-10ng/ml. In this “grey zone” range, only 20-25% of men will actually be found to have cancer.
However, as the PSA alone cannot diagnose cancer, most of these men will be directed to have a prostate biopsy to either definitively diagnose or exclude the presence of prostate cancer.


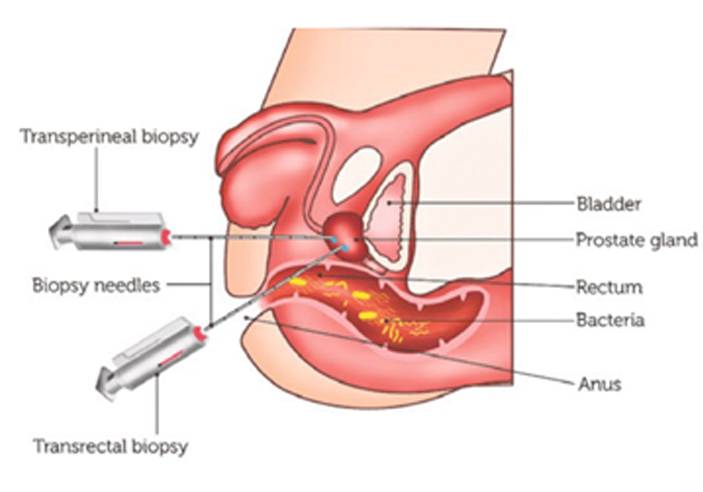
Prostate Biopsies Come with Risks
Prostate biopsies do come with risks of their own. They may result in complications such as blood in the urine and semen, infections which can be serious, and cause difficulty passing urine — requiring a catheter (urinary retention).
To do more good and reduce risks, we use additional measures to improve our risk stratification, so that only men with significant risk of harbouring prostate cancer are directed to have biopsies, and men at low risk, to avoid biopsies where possible.
Additional Measures Prior to Any Biopsy
The Prostate Health Index (phi) is a calculation that uses a combination of three blood tests to produce a "phi score." This score provides more information about what elevated PSA levels might mean and the probability of finding prostate cancer on biopsy. The phi has been shown to be 3x more accurate than the PSA in predicting that a biopsy will find prostate cancer.
Dr Lincoln Tan published the first local study on the phi in our local population, validating its effectiveness in minimising unnecessary biopsies.( Prospective validation of %p2PSA and the Prostate Health Index, in prostate cancer detection in initial prostate biopsies of Asian men, with total PSA 4-10 ng ml -1. Asian J Androl. 2017 May-Jun;19(3):286-290.).
MRIs in Predicting Risks
Magnetic Resonance Imaging (MRI) of the prostate has shown to be useful in predicting the risk of prostate cancer. However, the test is not perfect, and up to 15% of clinically significant cancers can still be missed with an MRI.
More accurate results come from centres with experienced radiologists specialized in reading prostate MRIs.
Which Test is the Most Accurate Then?
No one test is specific enough to exclude prostate cancer.
At Tan Urology, for men at risk of prostate,
we utilize a combination of personal risk factors, the phi score and the prostate MRI to determine each man’s individualised risk for harbouring prostate cancer. In this way, we avoid submitting men at low risk to unnecessary biopsies, yet not missing men with higher risks of having prostate cancer.
Dr Lincoln Tan has given talks on how to better risk stratify men for prostate biopsies to his urology colleagues both locally and overseas.
What happens if I am assessed to be at significant risk of prostate cancer?
For men assessed to be at intermediate or high risk of having prostate cancer, prostate biopsy will be recommended to obtain tissue samples to conclusively prove the presence or absence of cancer.
You can find out about our
safe and advanced technique of prostate biopsies here.






